Microsoft word - cv english.doc
CURRICULUM VITAE Starkenborglaan 6, 2341 BM, Oegstgeest, The Netherlands Telephone d . [email protected] Birthplace Date of Birth Marital Status Nationality EDUCATION Elementary School High School University University Leiden, The Netherlands, 1978-1983 Specializations Biochemistry, Physical Chemistry, Immunology, During specializations 3 publication
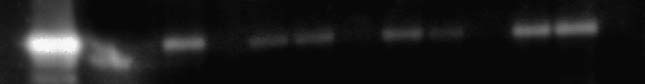 Fig. 2. Changes in endothelial nitric oxide synthase (eNOS) pro-
tein levels. A typical Western blot for eNOS in aortic tissue
with concentrations of eNOS (intensity units/50 mg tissue) in theleft ventricle of rats in heart failure (HF), with and without spiro-
nolactone treatment. First lane, eNOS-positive control; secondlane, HF treated with spironolactone; third and fourth lanes, un-
treated HF; and fifth lane, untreated sham. Note the decrease ineNOS protein levels in untreated HF compared with sham. Spiro-
nolactone treatment restored eNOS level similar to sham control.
Fig. 2. Changes in endothelial nitric oxide synthase (eNOS) pro-
tein levels. A typical Western blot for eNOS in aortic tissue
with concentrations of eNOS (intensity units/50 mg tissue) in theleft ventricle of rats in heart failure (HF), with and without spiro-
nolactone treatment. First lane, eNOS-positive control; secondlane, HF treated with spironolactone; third and fourth lanes, un-
treated HF; and fifth lane, untreated sham. Note the decrease ineNOS protein levels in untreated HF compared with sham. Spiro-
nolactone treatment restored eNOS level similar to sham control.