Goloy 33 eye care vitalize (der ultimative frische-kick für makellose augenpartien)
GOLOY 33 Eye Care Vitalize (new youthfulness around your eyes and the mouth) Water (as dissolver); together with hygroscopic agents; renders the subcorneous of the skin smooth, lissome and flexible Based on coconut; basic element of al fats and oils; hydrophilic; wetting agent Ester of coconut; gives higher elasticity and smoothness Texture maker from plants; emulsifier for O/W compounds P

 Prevention and Treatment of
Prevention and Treatment of 
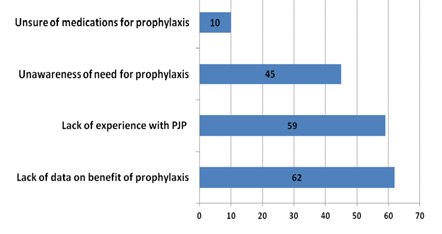 Risk Factors for PJP in IBD
Risk Factors for PJP in IBD